Digital Operating Room Summer School (DORS)
/ Leipzig, Germany
Due to the ongoing pandemic situation in Germany and the continuous lockdowns on federal and state levels, ICCAS is unfortunately unable to guarantee certainty this late summer in regards to the travel situation and access availability of our partner clinics. This makes the successful planning and organization of our annually held Digital Operating Room Summer School (DORS) nothing short of an impossible task. Thus, with a heavy heart, we have to announce the cancelation of this most anticipated event for 2021. However, ICCAS’ next Summer School will be hosted in summer 2022 and we are already accepting early registrations for it. We want to take this time to revise and refresh our concept for the DORS so we can host you again with an even stronger program next year! Stay tuned for updates!
Modern medical treatment is characterized by an increasing number of various technological elements such as technical medical instruments, medical information systems, imaging components and surgical assistance systems. The need for research and development into new medical systems and networked applications for methods of treatment is growing rapidly. This applies in particular to the scientific fields of medicine, computer science, engineering and mathematics. If they are to support individual treatment for patients in the best way possible, new technologies have to be integrated into the clinical environment. Moreover, these systems need to be able to communicate and interact both with each other and with the hospital’s IT system.
The integration of new technical infrastructure and technologies as well as the variety of resulting information present new challenges for physicians, engineers and manufacturers. To empower a new generation of young scientists to meet these challenges and carry out future projects, the Innovation Center Computer Assisted Surgery (ICCAS) at university Leipzig plans to hold its 8th Digital Operating Room Summer School (DORS) in 2022.
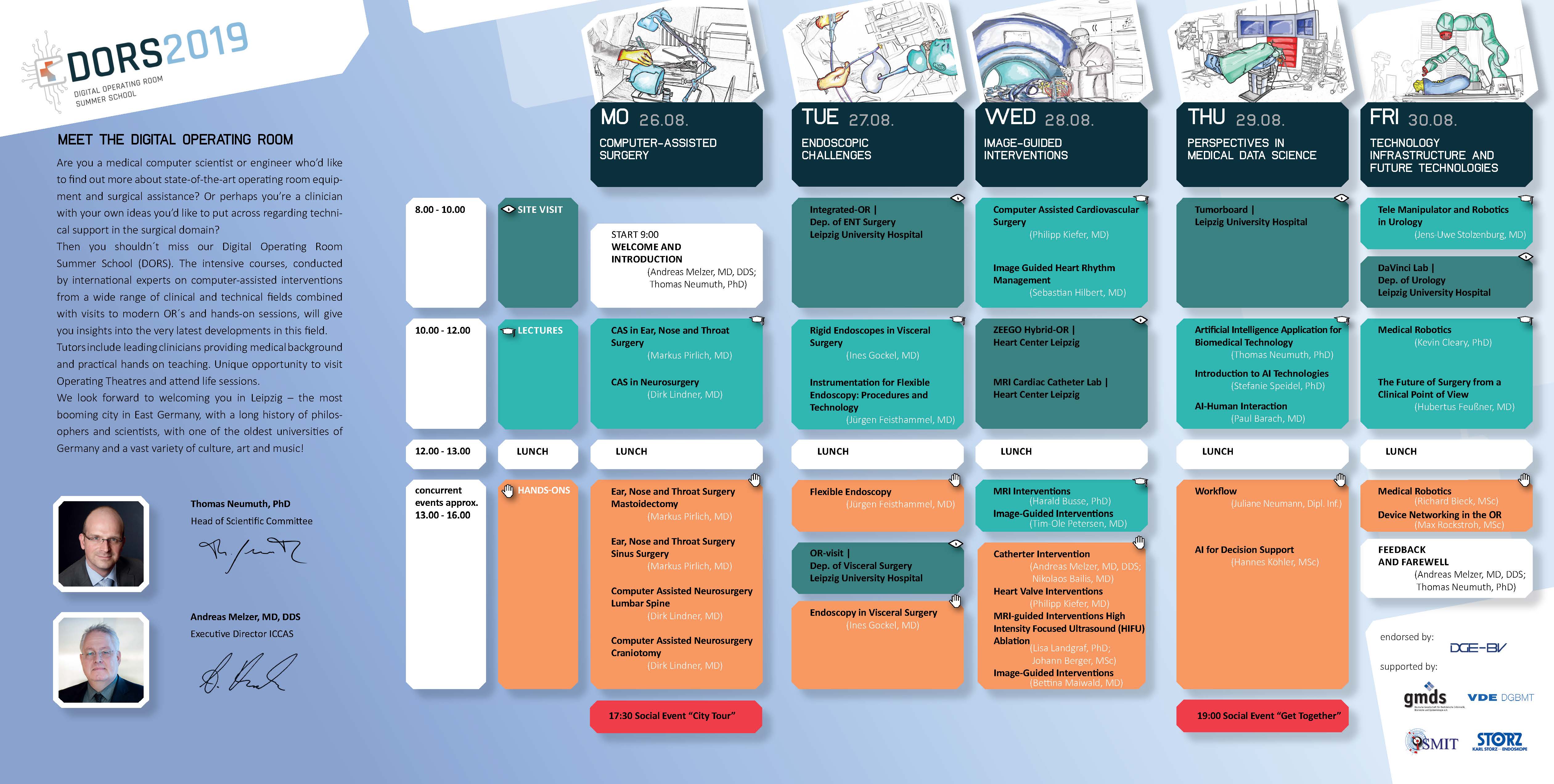
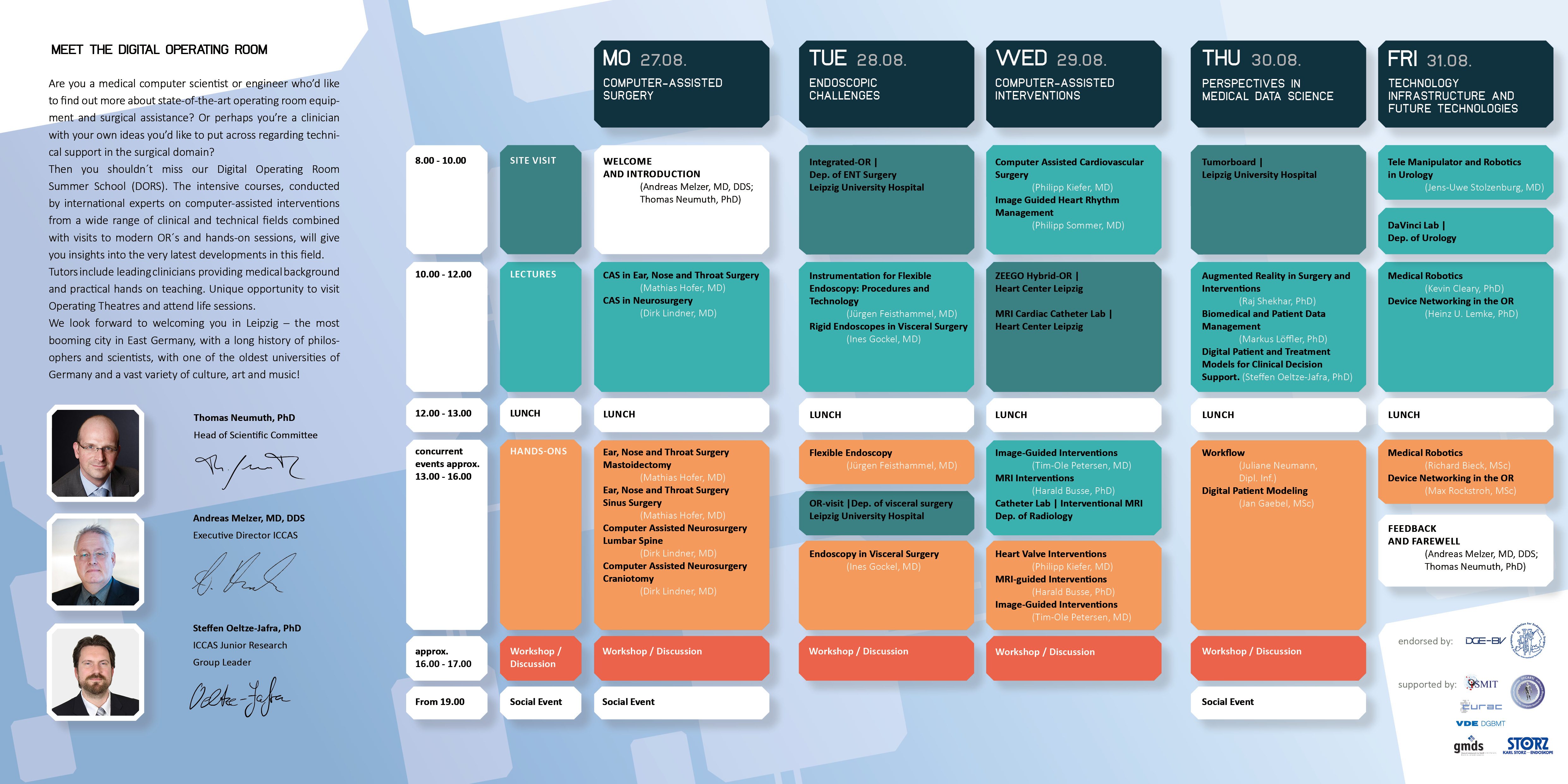
DORS is primarily aimed at graduates, doctoral students, post-docs and senior scientists from research and industry with a multidisciplinary background. The five-day intensive course with an attractive, varied program will comprise lectures, hands-on sessions, visits to operating rooms and individual workshops, giving the participants an extensive overview of medical technology in digital operating rooms from different angles along with insights into current research projects and problems.
Clinical experts and users will explain their views and expectations regarding innovative computer-assisted technologies as well as the current state of progress in clinical practice and research. Both successful developments and negative examples will be addressed and the advantages and disadvantages for therapeutic medicine set out. Moreover, the technical background of innovative infrastructure and technical standards will be examined, and various architectures, frameworks and communication technologies for computer assisted interventions in the digital operation room explained.
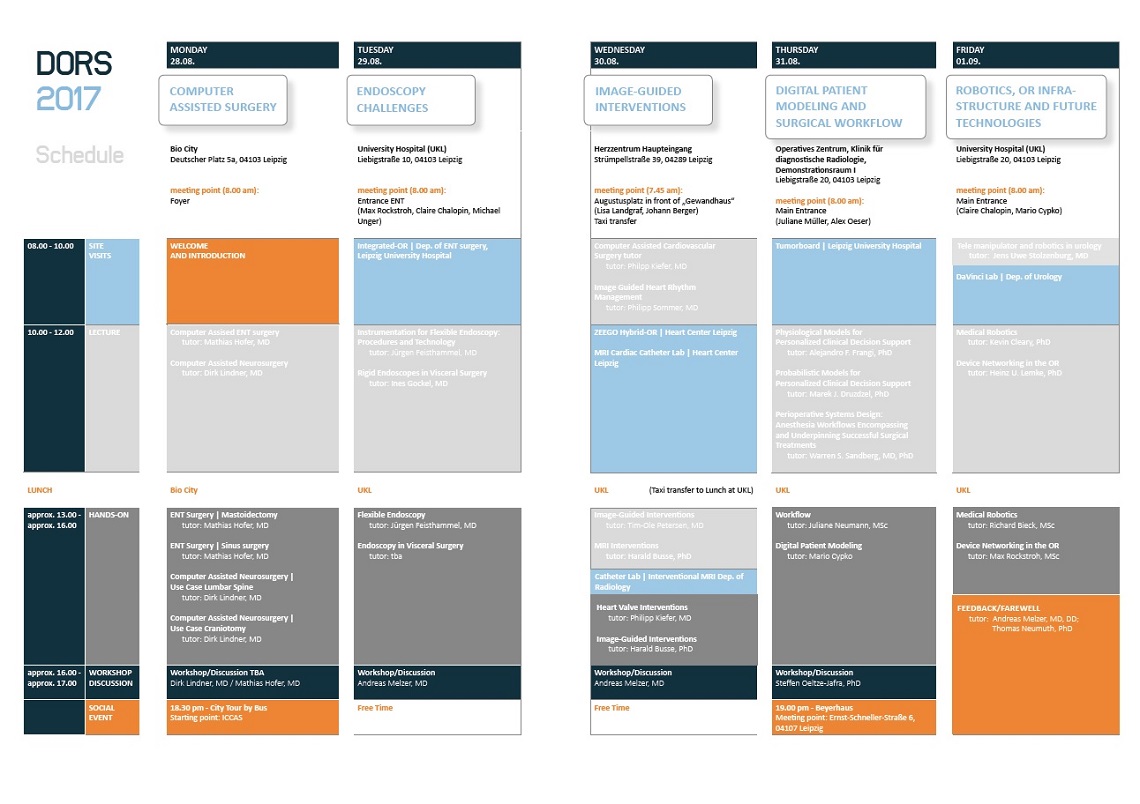
The educational concept of the summer school provides for the strong interdisciplinary dovetailing of medical and technical aspects in a manner which is unique in the global technology landscape. Accordingly, the summer school will be organized in daily modules each devoted to a different topic (see below) and divided into lectures, visits and hands-on sessions. In addition it is also planned to establish workshops, in which the participants put their own research fields under discussion.
This broad combination of teaching methods involving the close integration of theory and practice will give participants an intensive insight into many different aspects of computer-assisted surgery. Particular attention will be paid to achieving a sound balance between theoretical teaching, opportunities for participants to try out what they have learned, providing demonstrations of clinical practice and as individual workshops.
Planned practical demonstrations will take place at the following laboratories and operating rooms:
The educational concept of the summer school provides a strong interdisciplinary interaction of medical and technical aspects in a manner which is unique in the global technology landscape. Accordingly, the summer school will be organized in modules each devoted to a different topic and divided into lectures, visits and hands-on sessions.
This broad combination of teaching methods involving the close integration of theory and practice will give participants an intensive insight into many different aspects of computer-assisted surgery. Particular attention will be paid on achieving a sound balance between theoretical teaching and providing demonstrations of clinical practice.
 Computer Assisted Surgery (CAS)
Computer Assisted Surgery (CAS)
 Group photo, Computer Assisted Surgery (CAS)
Group photo, Computer Assisted Surgery (CAS)
 Endoscopic Challenges
Endoscopic Challenges
 Endoscopic Challenges
Endoscopic Challenges
 Endoscopic Challenges
Endoscopic Challenges
 Endoscopic Challenges
Endoscopic Challenges
 Image-Guided Interventions
Image-Guided Interventions
 Digital Patient Modeling and surgical Workflow
Digital Patient Modeling and surgical Workflow
 Robotics, OR Infrastructure and Future Technologies
Robotics, OR Infrastructure and Future Technologies
 Robotics, OR Infrastructure and Future Technologies
Robotics, OR Infrastructure and Future Technologies
 Robotics, OR Infrastructure and Future Technologies
Robotics, OR Infrastructure and Future Technologies
 Robotics, OR Infrastructure and Future Technologies
Robotics, OR Infrastructure and Future Technologies
 Computer Assisted Surgery (CAS)
Computer Assisted Surgery (CAS)
 Computer Assisted Surgery (CAS)
Computer Assisted Surgery (CAS)
 Computer Assisted Surgery (CAS)
Computer Assisted Surgery (CAS)
 Endoscopic Challenges
Endoscopic Challenges
 Endoscopic Challenges
Endoscopic Challenges
 Image-Guided Interventions
Image-Guided Interventions
 Image-Guided Interventions
Image-Guided Interventions
 Image-Guided Interventions
Image-Guided Interventions
 Digital Patient Modeling and Surgical Workflow
Digital Patient Modeling and Surgical Workflow
 Digital Patient Modeling and Surgical Workflow
Digital Patient Modeling and Surgical Workflow
 Robotics, OR Infrastructure and Future Technologies
Robotics, OR Infrastructure and Future Technologies
 Group photo; Robotics, OR Infrastructure and Future Technologies
Group photo; Robotics, OR Infrastructure and Future Technologies
ICCAS‘s Digital Operating Room Summer School (DORS) successfully ended in early September. The feedback of the 26 participants from 12 states was very positive. They were convinced by the well balanced combination of theoretical knowledge transfer, OR-visits and practical units. Physicians of Leipzig University Hospital and Heart Center Leipzig as well as foreign experts supported the extensive summer school program, certified with 38 European CME-Credits (EACCME®). The course contents included computer assisted applications in the fields of ENT-, Neuro-, Visceral- and Heart-surgery, Urology and Radiology, the Digital Patient Model, medical robotics and technologies for the future operating room. The next DORS is scheduled from August 27 – 31, 2018.
 DORS-Team - Participants and tutors all together
DORS-Team - Participants and tutors all together
 Dirk Lindner, MD - Introduction in hands-on Neurosurgery
Dirk Lindner, MD - Introduction in hands-on Neurosurgery
 Harald Busse, PhD - Shows a setup of image guided intervention in Department of radiology
Harald Busse, PhD - Shows a setup of image guided intervention in Department of radiology
 Mario Cypko, PhD - Supports hands-on Digital Patient Modeling
Mario Cypko, PhD - Supports hands-on Digital Patient Modeling
 Participant - Hands-on ENT-surgery
Participant - Hands-on ENT-surgery
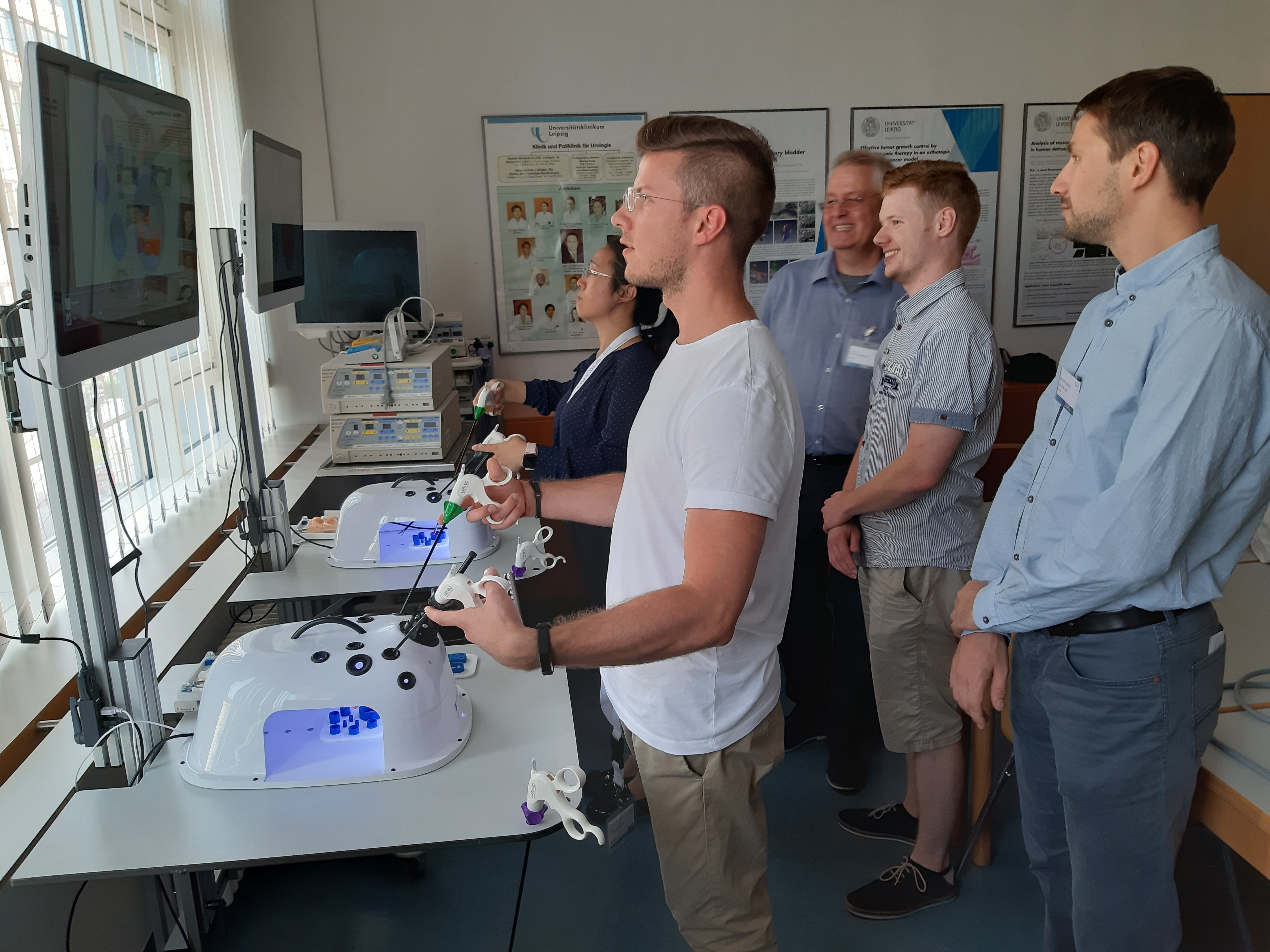
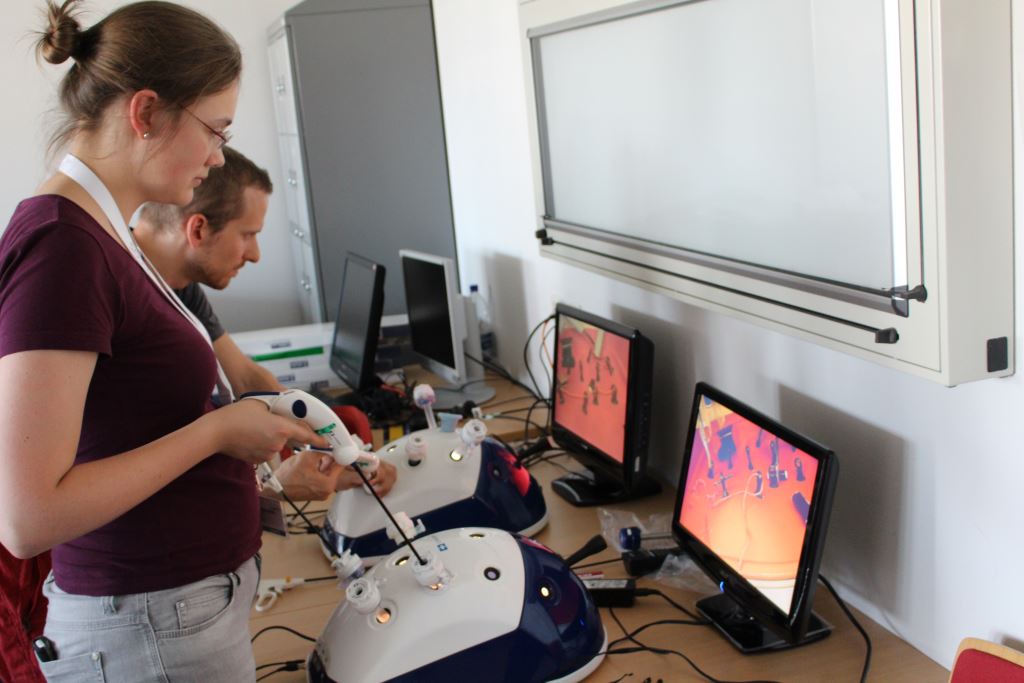
 Participants - Hands-on in surgical robotics
Participants - Hands-on in surgical robotics
 Prof. Andreas Melzer, MD, DD and Juergen Feisthammel, MD - Lecture in Endoscopy
Prof. Andreas Melzer, MD, DD and Juergen Feisthammel, MD - Lecture in Endoscopy
 Prof. Kevin Cleary, PhD - Lecture in Medical Robotics
Prof. Kevin Cleary, PhD - Lecture in Medical Robotics
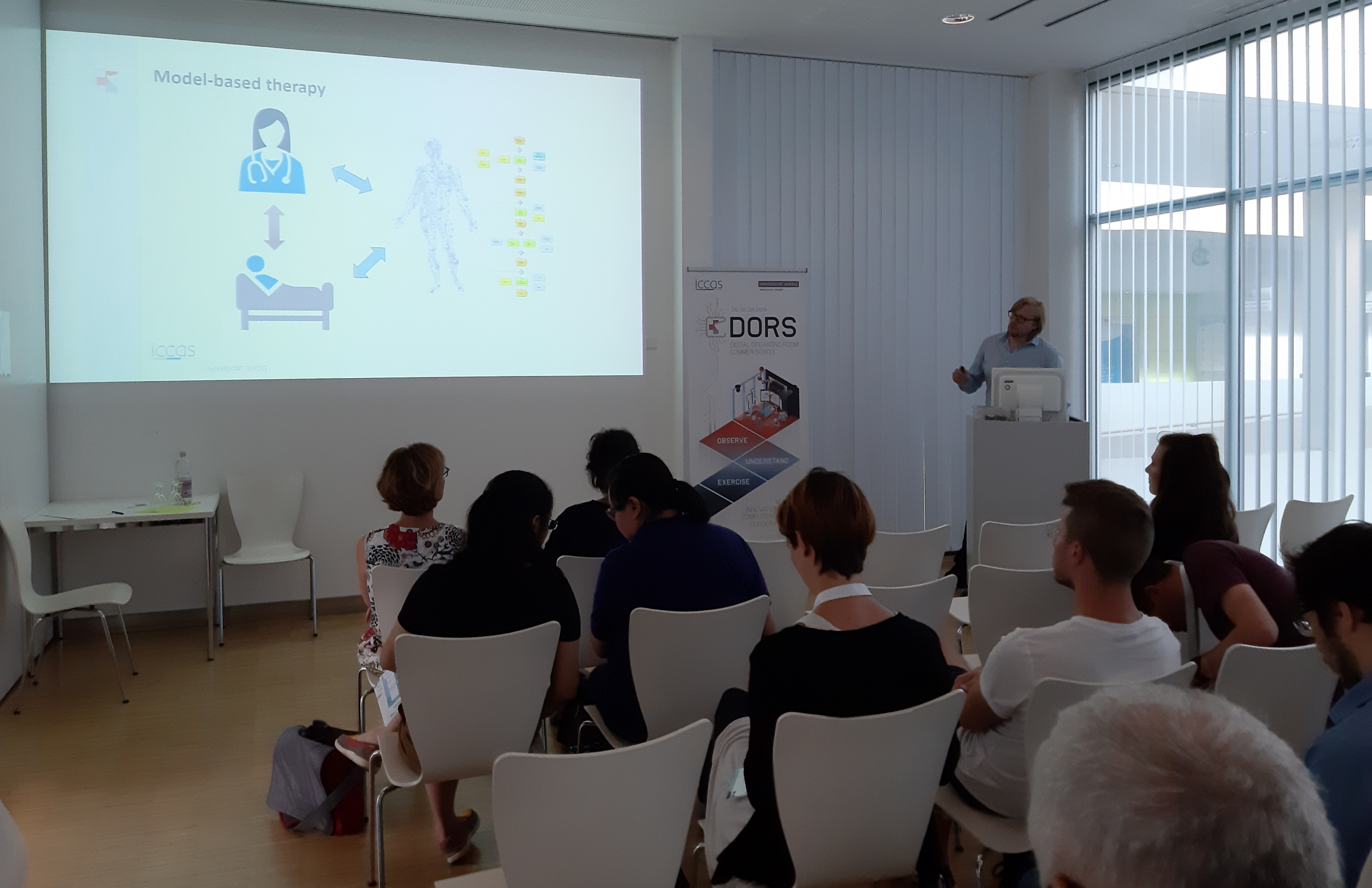
 Prof. Thomas Neumuth, PhD - Welcome and Introduction
Prof. Thomas Neumuth, PhD - Welcome and Introduction
 Stefan Franke, PhD - Introduction in hands-on OR-workflows
Stefan Franke, PhD - Introduction in hands-on OR-workflows

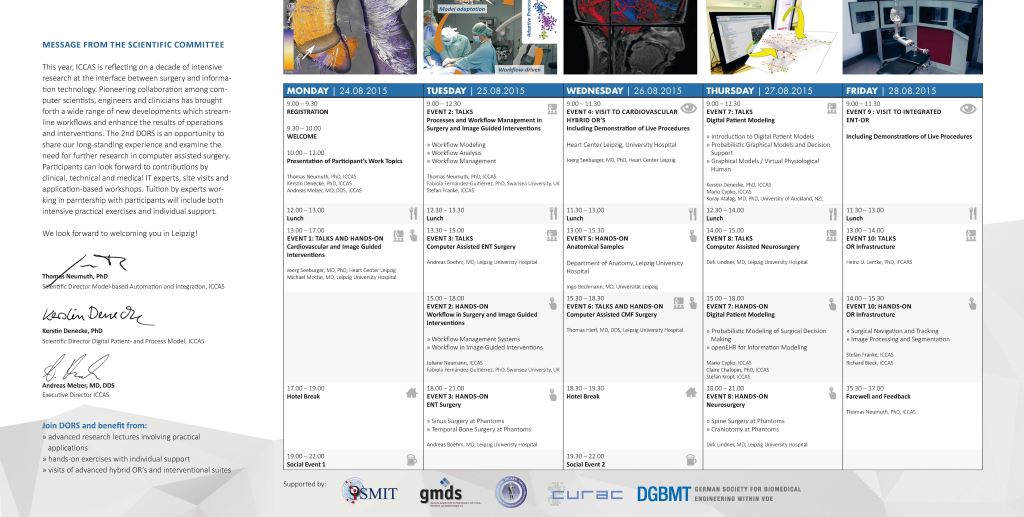
The internationally oriented course familiarized about 20 participants latest computer-assisted OR-technolgy from the object of research until the direct use on the patient.
Computer scientists, engineers and medics from Germany, Switzerland, the Netherlands, Turkey, Italy, China, Japan and India experienced an inspiring week with many practical sessions. The well filled programm kept its promise – interesting expert lectures, followed by practical exercises partly on patient phantoms and visits to state-of-the-art operating theaters and labs of Leipzig University Hospital and Heart Center Leipzig.
The participants praised the good balance between clinical and technical aspects as well as the theoretical explanations and practical sessions. The whole course was certified with 57 credits by the national authority ‘Sächsische Landesärztekammer’ and with 33 European CME-credits (EACCME®).
 Prof. Neumuth - Welcome and Introduction
Prof. Neumuth - Welcome and Introduction
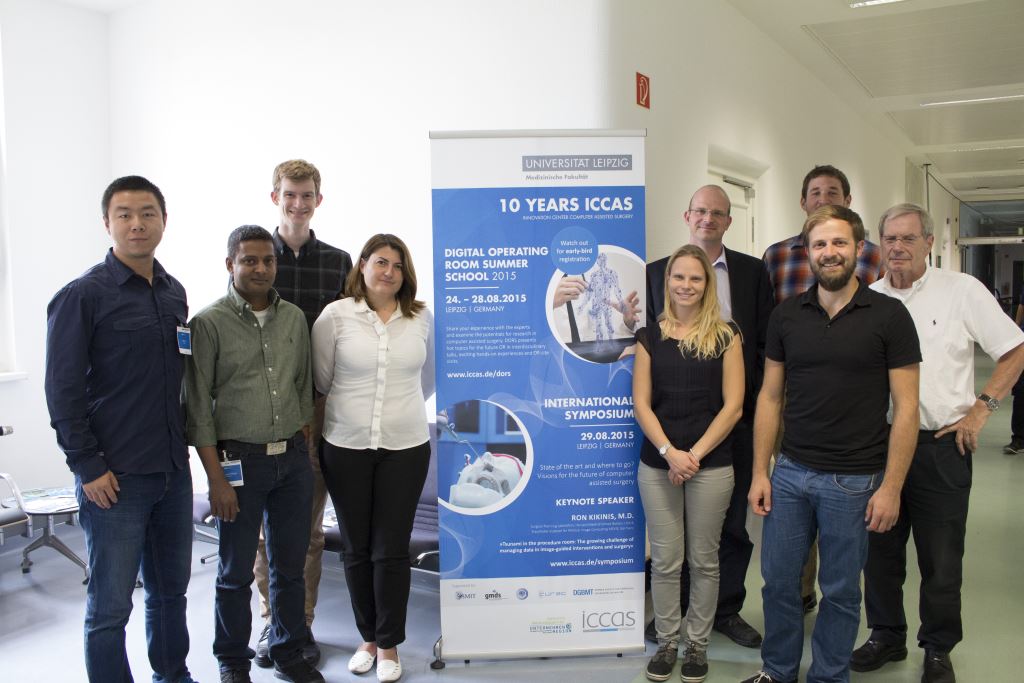
 Participants and tutors all together
Participants and tutors all together
 Dirk Lindner, MD - supports hands-on CAS in Neurosurgery
Dirk Lindner, MD - supports hands-on CAS in Neurosurgery
 Prof. Alberto Arezzo - supports hands-on Flexible Endoscopy
Prof. Alberto Arezzo - supports hands-on Flexible Endoscopy
 Gero Kraus, MSc - supports hands-on Surgical Robotics
Gero Kraus, MSc - supports hands-on Surgical Robotics
 Salih Abdelaziz, PhD - lecture about Surgical Robotics
Salih Abdelaziz, PhD - lecture about Surgical Robotics
 Participants - hands-on training an Aortic Valve Implantation
Participants - hands-on training an Aortic Valve Implantation
 Participants - hands-on training on Laparoscopy Trainer (Lübecker Tool Box)
Participants - hands-on training on Laparoscopy Trainer (Lübecker Tool Box)
 Prof. Thomas Neumuth - Welcome and Introduction
Prof. Thomas Neumuth - Welcome and Introduction
 Participants and tutors
Participants and tutors
 Visit to integrated ENT-OR
Visit to integrated ENT-OR
 Dirk Lindner, MD - introduction hands-on Neurosurgery
Dirk Lindner, MD - introduction hands-on Neurosurgery
 Dirk Lindner, MD - supports hands-on Neurosurgery
Dirk Lindner, MD - supports hands-on Neurosurgery
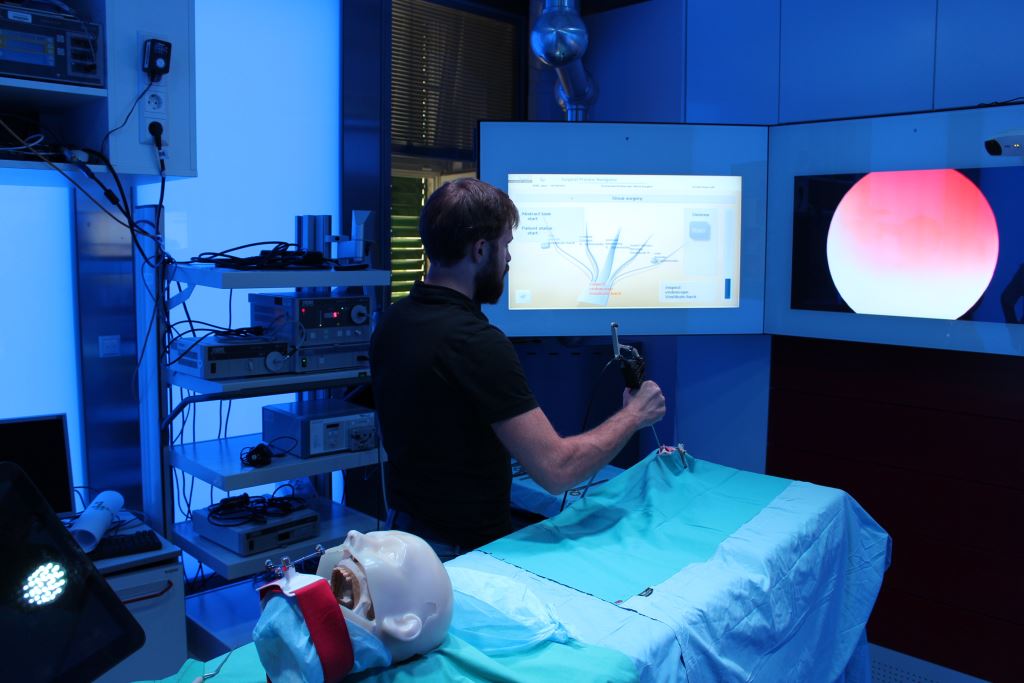 Participant at ICCAS Demo OR
Participant at ICCAS Demo OR
Application is open to:
from the fields of
| TYPE | Early-bird | Regular | per module |
|---|---|---|---|
| M.Sc./ PhD students | 600 € | 700 € | 300 € |
| Academic position | 900 € | 1.000 € | 300 € |
| other participants | 1.200 € | 1.200 € | 300 € |
The school will be held at the premesis of ICCAS (Semmelweisstrasse 14, 01403 Leipzig).
Leipzig is always worth a visit. The city of Linden, is now over a thousand years old and Germany's fastest growing city. Famous events in European history such as the Battle of Leipzig in 1813 and the Peaceful Revolution in 1989 are associated with it. Today, Leipzig is a key center of commerce, culture and learning. Moreover, the city has become an attractive business location in Central Germany. It focuses on expanding industries such as biotech and biomedical engineering. The result is an extended landscape of higher education and the establishment of important research centers. After work a guided tour through Leipzig city center or a pub visit are planned to better get to know the location and your international colleagues.
We look forward to welcoming you!
Prof. Thomas Neumuth, PhD | ICCAS vice director
E-Mail: thomas.neumuth@medizin.uni-leipzig.de
Prof. Andreas Melzer, MD, DDS | ICCAS director
E-Mail: andreas.melzer@medizin.uni-leipzig.de
Event organization
Universität Leipzig // Faculty of Medicine
Innovation Center Computer Assisted Surgery (ICCAS)
Frederik Krabbes
Phone: 0341 / 97-12032
Fax: +49( (0) 341 / 97 12009
E-Mail: dors@iccas.de